
How Gum Health Influences Erectile Dysfunction
Literature reviews suggest a possible relationship between periodontal diseases and various conditions such as cardiovascular issues, stroke, diabetes, low pregnancy outcomes, gastrointestinal problems, respiratory diseases, osteoporosis, erectile dysfunction, and kidney disorders (1).
Periodontal diseases are generally divided into gingivitis and periodontitis. Gingivitis is described as an inflammatory condition affecting only the gums without damage to the supporting tissues. Periodontitis is an inflammatory disease resulting from the interaction between dental plaque and the host, damaging not only the gums but also the periodontal ligament and alveolar bone.
In this blog post, we will discuss the interaction between gum diseases and the respiratory system.
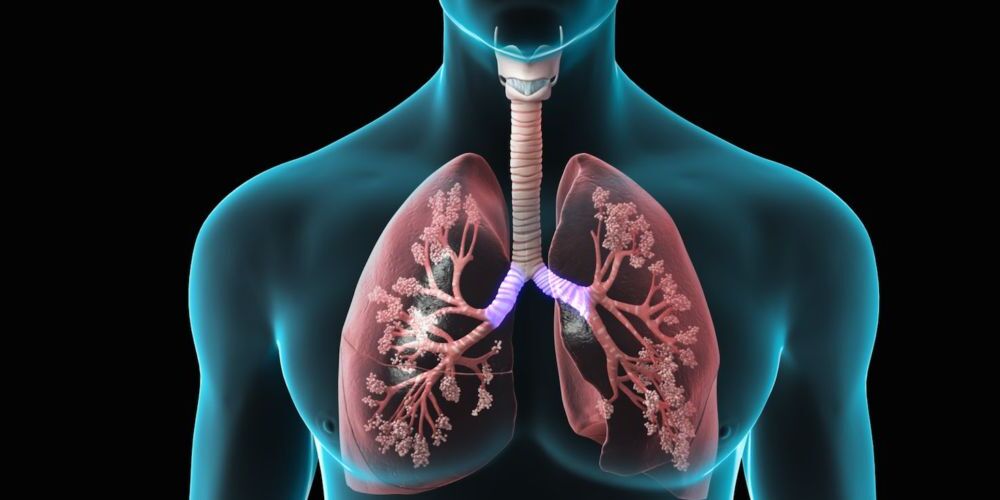
Periodontal Diseases and Respiratory Disorders
Periodontal diseases have been shown to have a bidirectional relationship with many systemic diseases. Recent studies have explored the potential links between respiratory and periodontal disorders, generally indicating a positive correlation between the two (1).
The connection between lung diseases and gum diseases has been known for a long time. Due to the anatomical relationship between the oral cavity and the respiratory tract, bacteria present in the mouth can be aspirated into the lower respiratory tract, leading to inflammation.
Some studies have shown that:
- In intensive care patients, bacteria from the mouth have been observed to infect the lungs.
- During the pandemic, it has been found that individuals with gum disease who contracted COVID-19 were 3.5 times more likely to be admitted to intensive care and 4.5 times more likely to require ventilation.
- COVID-19 has presented some oral symptoms in recent research. Saliva may serve as a reservoir for pathogenic bacteria. A literature review has highlighted that COVID-19 can manifest as ulcers, erosions, blisters, vesicles, changes in the surface of the tongue, pigmentation, halitosis, whitish areas, necrosis, and spontaneous bleeding (1).
Periodontal Diseases and Erectile Dysfunction
Interestingly, recent studies have begun to explore the correlation between periodontal diseases and erectile dysfunction, further highlighting the systemic impact of oral health. Research suggests that periodontal disease, as a chronic inflammatory condition, may contribute to vascular dysfunction, which is a common cause of erectile dysfunction. The inflammation caused by gum disease can lead to endothelial dysfunction in blood vessels throughout the body, including those leading to the penile region, impairing blood flow and contributing to the occurrence of erectile dysfunction.
Studies indicate that men with periodontal disease are more likely to experience erectile dysfunction compared to those with healthy gums. This relationship underscores the importance of maintaining excellent oral hygiene not only for overall health but also as a preventative measure against erectile dysfunction. Addressing periodontal disease through regular dental check-ups, proper brushing, and flossing, and potentially seeking treatment can have beneficial effects beyond the mouth, possibly improving erectile function and overall vascular health.
Treatment Methods for Periodontal (Gum) Diseases
The treatment for gum diseases can vary depending on the severity, type of the disease, and the patient’s overall health condition. However, the following treatment methods can be used:
– Professional Dental Cleaning: Removal of tartar and plaque by a dentist is a fundamental step in controlling gum diseases.
– Tartar Removal (Scaling): Involves cleaning tartar accumulated under the gum line and on the teeth surfaces. Tartar is a primary cause of gum inflammation.
– Non-surgical periodontal treatments (subgingival curettage) include Root Surface Smoothing (Root Planing): This procedure smoothens and cleans the teeth root surfaces to halt disease progression and promote healing. It is performed under local anesthesia and may involve local antibiotics, systemic antibiotics, host modulators, and dental lasers.
– Surgical Treatments: Advanced cases of gum disease or cases not responding to other treatments may require surgical intervention. This involves removing the gum to clean all inflammatory tissues and bacteria residues in the root pocket, possibly followed by regenerative procedures depending on the extent of bone damage.
– Regenerative methods are surgical periodontal treatments using membranes, bone grafts, or tissue-stimulating proteins to clean the root surface and surrounding inflamed tissues.
– Antibiotic Therapy: For severe gum diseases, doctors may recommend local or systemic antibiotics to help control infections.
– Home Care: Treatment requires regular oral hygiene practices at home, including brushing, flossing, and using antiseptic mouthwash.
– Regular Follow-ups and Maintenance: It’s crucial to continue seeing your dentist regularly after treatment to maintain gum health and prevent disease recurrence. Lifetime adherence to periodontal control appointments set by your dentist is necessary to prevent relapse.
In conclusion, since every patient is different, the treatment plan should be tailored to the individual. It’s important to work with your dentist to determine the most
appropriate treatment plan. Remember, oral health is not just about a beautiful smile; it’s also about leading a healthy life.
References:
1- PERIODONTAL AND SYSTEMIC DISEASES: RESPIRATORY DISORDERS by Hasan HATİPOĞLU, Kütahya Health Sciences University, Faculty of Dentistry, Department of Periodontology, Kütahya, Turkey
2- DOI references: 10.1902/jop.2012.120399, DOI: 10.2147/COPD.S327036, DOI: 10.1111/jcpe.12247, DOI: 10.1111/jcpe.13287, DOI: 10.1111/jcpe.13886.
