
Jaw Bone Resorption and Implants: What You Need to Know
Jaw bone resorption is a natural bone loss process where the jawbone gradually breaks down, often triggered by tooth loss, gum disease, or other factors. This condition can significantly alter facial aesthetics, leading to a shrinking jaw and changes in facial structure. The impact extends beyond appearance, affecting functionality with challenges in chewing and speaking.
Understanding jaw bone resorption is crucial for effective treatment planning. As the jawbone loses density and volume, it risks compromising oral health and overall quality of life. Recognizing the signs early can guide timely intervention and prevent further complications.
Dental implants emerge as a popular solution for addressing jaw bone resorption. They not only restore missing teeth but also play a vital role in maintaining the structural integrity of the jawbone. By simulating natural tooth roots, implants stimulate the underlying bone, preventing further deterioration. This dual benefit makes dental implants an appealing choice for those experiencing jaw bone loss—restoring both appearance and function.
If you or someone you know is facing issues related to jaw bone resorption or missing teeth, consider scheduling a consultation at Fine Up Clinic for expert advice and treatment options.

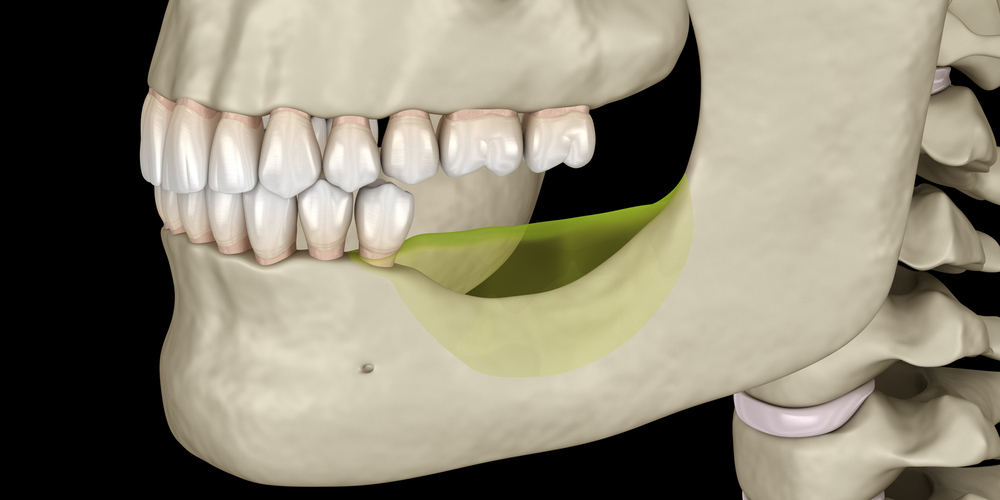
Bone loss progresses over time, affecting both the structure and function of the jaw.
Understanding Jaw Bone Resorption
Jaw bone resorption is a natural process that involves the gradual breakdown of bone tissue in the jaw. This condition progresses over time, affecting both the structure and function of the jaw. Without intervention, it can lead to significant dental and facial changes.
Osteoclasts: The Key Players
Osteoclasts are specialized cells responsible for breaking down bone tissue. In jaw bone resorption, these cells target the alveolar bone, which surrounds and supports teeth. As osteoclasts become more active, they reduce the density of the alveolar bone, causing a loss of support for dental structures.
The Role of Alveolar Bone
The alveolar bone is crucial for maintaining tooth stability. When this bone deteriorates, teeth lose their anchoring support, leading to mobility and potential tooth loss. The weakening of this bone doesn’t only affect teeth but also jeopardizes overall jaw integrity.
Bone Remodeling: A Balancing Act
Bone remodeling is an ongoing process where old bone is removed and new bone is formed. It’s essential for maintaining healthy jawbone density. Here’s how it works:
- Resorption Phase: Osteoclasts break down old or damaged bone tissue.
- Formation Phase: Osteoblasts (bone-forming cells) create new bone material, restoring strength and density.
This dynamic balance ensures the structural stability of bones throughout life. However, when resorption outpaces formation—often due to factors like missing teeth or periodontal disease—jawbone density decreases.
Importance of Healthy Jawbone Density
Maintaining healthy jawbone density is crucial for:
- Facial Structure: Jawbone supports facial muscles and skin; loss leads to sunken cheeks and altered appearance.
- Functionality: Strong bones are necessary for chewing and speaking without discomfort or difficulty.
- Oral Health: Dense bones provide a foundation for effective dental treatments such as implants or bridges.
Understanding the intricacies of jaw bone resorption highlights its impact on dental health and aesthetics. This knowledge lays the groundwork for exploring treatment options that address these challenges effectively.
Causes, Symptoms, and Impact on Oral Health
Jaw bone resorption is often triggered by several common factors that undermine oral health. Understanding these causes can aid in early identification and treatment.
Causes of Jaw Bone Resorption
- Tooth Loss: Whether due to decay or trauma, missing teeth significantly contribute to bone resorption. Teeth provide necessary stimulation to the jawbone. When teeth are absent, the lack of stimulation leads to atrophy.
- Periodontal Disease: This gum disease is a major culprit affecting jawbone integrity. As periodontal disease progresses, it destroys the supporting tissues of the teeth, leading to bone loss.
- Tooth Extraction: Although sometimes necessary, tooth extraction can accelerate jaw bone resorption if not followed by timely restorative procedures like implants.
Symptoms of Jaw Bone Loss
Detecting the symptoms early can prevent further complications:
- Changes in Bite Alignment: As the jawbone deteriorates, it affects how teeth align with each other, leading to an uncomfortable bite and misalignment issues.
- TMJ Pain: The temporomandibular joint may become strained due to changes in bite or structure, causing pain or discomfort around the jaw.
Impact on Oral Health
Compromised jaw support manifests in various functional challenges:
- Chewing Difficulties: A weakened jawbone struggles to support normal chewing functions, limiting dietary options and impacting nutrition.
- Speech Impairment: Jawbone stability plays a crucial role in clear speech articulation. Bone loss may lead to slurred or impaired speech.
It’s essential to address these issues promptly. Recognizing the signs and understanding the underlying causes can guide effective treatment strategies, helping maintain both oral function and aesthetics.
Moreover, it’s important to note that oral health doesn’t exist in isolation. There is a significant connection between dental health and overall systemic health, including heart health. Therefore, maintaining optimal oral health is crucial not only for preserving dental function but also for safeguarding overall health.
The Role of Dental Implants in Combating Jaw Bone Resorption
Dental implants are a game-changing solution for people dealing with jaw bone resorption. These implants, designed to imitate the structure and function of natural tooth roots, do more than just replace missing teeth—they also provide essential stimulation to the underlying jawbone. This stimulation is crucial in preventing further resorption and maintaining bone density over time.
How Do Dental Implants Work?
1. Replacement and Stimulation
Unlike traditional dentures or bridges, dental implants are securely anchored directly into the jawbone. This anchorage not only ensures stability for artificial teeth but also delivers the necessary mechanical stimulation to the jawbone. Without this engagement, the bone can continue to deteriorate.
2. Preventing Further Resorption
The presence of an implant plays a significant role in maintaining the structural integrity of the jaw. As it integrates with the bone, it functions like a natural tooth root, providing vital support and preventing atrophy.
The Significance of Osseointegration
A key factor in the success of dental implants is osseointegration—the biological process through which the implant fuses with the surrounding bone tissue.
1. Long-term Success and Stability
Osseointegration is critical for ensuring that the implant becomes a permanent part of the mouth’s anatomy. This fusion process typically takes several months, during which new bone cells grow around the titanium post, securing it firmly in place.
2. Enhanced Oral Functionality
Once fully integrated, implants restore complete chewing power and comfort similar to natural teeth. This stability further supports facial aesthetics by preventing shifts in other teeth and preserving facial structure.
Dental implants go beyond being mere cosmetic solutions; they are vital instruments in fighting against jaw bone resorption. By encouraging natural-like interactions within the mouth, they promote both oral health and overall well-being.
Exploring Alternative Implant Solutions for Severe Cases
In situations where traditional dental implants aren’t feasible due to significant jawbone loss, alternative implant solutions such as zygomatic implants and mini implants provide effective options.
When Are Alternative Implant Solutions Necessary?
Alternative implant solutions become necessary in the following situations:
- Severe Bone Resorption: When jawbone density is too low for standard implants, alternative solutions become essential.
- Complex Anatomical Structures: Patients with unique oral structures that complicate conventional implant placement may benefit from these alternatives.
- Previous Implant Failures: Individuals who have experienced failed implants might find success with these specialized options.
Benefits of Zygomatic Implants
Zygomatic implants are longer than traditional ones and anchor into the cheekbone (zygomatic bone) rather than the maxillary bone. This makes them ideal for:
- Patients with Severe Maxillary Bone Loss: They bypass the need for bone grafting by securing directly to the cheekbone.
- Immediate Functionality: Often allow for immediate loading, meaning temporary teeth can be placed on the same day as surgery.
- Enhanced Stability: The anchorage in denser bone provides robust support.
Advantages of Mini Implants
Mini implants are smaller in diameter and offer a less invasive solution compared to regular implants. Their benefits include:
- Minimal Bone Requirement: Suitable for patients with limited bone available without the need for extensive augmentation procedures.
- Quicker Recovery Time: Less invasive nature leads to faster healing and reduced discomfort post-surgery.
- Cost-Effective Option: Typically more affordable than traditional implants, making them an attractive option for many patients.
These innovative implant solutions expand possibilities for individuals facing severe jawbone challenges, restoring not only function but also confidence in their smiles. By offering tailored approaches like zygomatic and mini implants, dental professionals can better address diverse patient needs, ensuring optimal outcomes even in complex cases.
Considerations Before Undergoing Implant Surgery
Preparing for dental implant surgery involves understanding what happens during the procedure, the expected recovery time, and the importance of adhering to post-operative instructions.
What to Expect During Surgery
- Procedure Duration: Dental implant surgery typically takes about 1-2 hours per implant.
- Anesthesia Options: Local anesthesia is commonly used, though sedation may be available for patients with anxiety.
- Surgical Steps:
- Incision in the gum to expose the bone.
- Drilling a hole into the jawbone where the implant will be placed.
- Insertion of the titanium implant post, which acts as a root replacement.
Recovery Time After Surgery
- Initial Healing Phase: Usually spans 1-2 weeks. Patients may experience swelling, bruising, and minor bleeding.
- Osseointegration Period: The process where the jawbone fuses with the implant can take several months (typically 3-6 months) before the final crown is attached.
Post-Surgery Recovery Tips
- Follow-Up Appointments: Regular check-ups ensure proper healing and integration.
- Oral Hygiene Practices: Maintain cleanliness around the surgical site to prevent infection.
- Dietary Adjustments: Soft foods are recommended initially to avoid pressure on the implant.
Adhering strictly to post-operative care instructions is crucial for successful healing and long-term stability of dental implants. Skipping any step could affect both recovery time and overall outcomes.
Managing Pain Associated with Jaw Issues Post-Implantation
Pain management for jaw issues is a crucial aspect of recovery following dental implant procedures. Addressing discomfort effectively ensures a smoother healing process and enhances patient comfort.
Strategies for Managing Pain:
- Medication: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, are often recommended. In some cases, your healthcare provider might prescribe stronger medications.
- Cold Compresses: Applying a cold compress to the affected area can help reduce swelling and numb pain.
- Rest and Elevation: Keeping your head elevated when lying down can minimize swelling and discomfort.
- Soft Diet: Consuming soft foods reduces strain on the jaw during chewing, which can alleviate pain.
Role of Healthcare Providers:
Healthcare providers play a vital role in pain management for jaw bone resorption post-implantation. They offer:
- Personalized Pain Management Plans: Tailored strategies based on individual needs and pain thresholds.
- Monitoring and Adjustments: Regular follow-ups to assess pain levels and adjust treatments as necessary.
- Guidance and Support: Professional advice on managing side effects and ensuring optimal recovery.
Understanding these strategies not only aids in effective pain management but also contributes to the overall success of dental implant procedures by promoting a comfortable healing environment.
A dental bone graft operation involves transplanting bone tissue to the jawbone to support dental implants or restore bone loss caused by tooth extractions or periodontal disease.
Preventive Measures Against Future Jaw Bone Resorption After Implant Placement
Ensuring the longevity of dental implants and preventing bone resorption after implant placement involves commitment to oral hygiene and regular dental care. Here are some effective strategies:
Maintain Rigorous Oral Hygiene
- Brush and Floss Regularly: Use a soft-bristled toothbrush and fluoride toothpaste to clean your teeth at least twice daily. Flossing helps remove food particles and plaque from areas your toothbrush can’t reach.
- Mouth Rinse: Consider using an antibacterial mouthwash to reduce plaque and prevent infection around the implants.
Regular Dental Check-Ups
- Routine Examinations: Schedule dental visits every six months. Your dentist will check the condition of your implants, assess bone density, and address any developing issues promptly.
- Professional Cleanings: These cleanings help remove tartar build-up that can’t be eliminated through regular brushing and flossing.
Healthy Lifestyle Choices
- Balanced Diet: Consuming a diet rich in calcium and vitamin D supports bone health. Incorporate dairy products, leafy greens, and fish into your meals.
- Avoid Tobacco Products: Smoking can hinder healing post-implantation and increase the risk of periodontal disease.
These practices not only safeguard against future complications but also reinforce the stability of your dental implants, ensuring they serve you well for years to come.
Taking Action Against Jaw Bone Resorption with Implants
Addressing jaw bone resorption promptly is crucial for maintaining both oral health and facial aesthetics. Early intervention with appropriate jaw bone resorption treatment options can significantly enhance outcomes.
Dental implants, a popular choice, offer a dual benefit: they restore function and prevent further bone loss by acting as artificial roots. The process of osseointegration ensures the stability and success of implants, making them an effective solution for many.
Why act now?
- Delaying treatment can lead to increased complications, like further bone loss and changes in facial structure.
- Seeking early solutions often means simpler procedures and better results.
Consulting a qualified professional is essential. At FineUp Clinic, our team provides personalized guidance tailored to your needs. We’re committed to helping you navigate your options effectively, ensuring the best possible care.
Taking action against jaw bone resorption is not just about restoring your smile; it’s about preserving your quality of life. Don’t wait—explore your treatment options today to safeguard your oral health for the future.
FAQs (Frequently Asked Questions)
What is jaw bone resorption and how does it affect facial aesthetics?
Jaw bone resorption is the progressive loss of bone density in the jaw, often resulting from missing teeth or periodontal disease. This condition can lead to noticeable changes in facial structure, including a sunken appearance and altered bite alignment, significantly impacting both aesthetics and functionality.
What are the common causes of jaw bone resorption?
Common causes of jaw bone resorption include missing teeth due to decay or trauma, periodontal disease that affects gum health, and tooth extractions that compromise jawbone integrity. Each of these factors can contribute to the gradual deterioration of alveolar bone surrounding the teeth.
How do dental implants help prevent further jaw bone resorption?
Dental implants serve as a restoration method that replaces missing teeth while stimulating the underlying jawbone. This stimulation is crucial in preventing further resorption, as it encourages osseointegration—the process by which the implant fuses with the surrounding bone—ensuring long-term success and stability.
What alternative implant solutions are available for severe cases of jaw bone loss?
In severe cases of jaw bone loss, alternative implant solutions such as zygomatic implants and mini implants may be necessary. These options provide benefits by anchoring implants in areas with adequate bone support, allowing for effective restoration even when traditional implants are not feasible.
What should I expect during recovery after dental implant surgery?
Recovery after dental implant surgery typically involves a healing period where you may experience some discomfort. It is important to follow post-operative care instructions provided by your healthcare provider to ensure proper healing. Recovery time can vary but generally lasts a few weeks before the full benefits of the implants are realized.
How can I manage pain associated with jaw issues after implantation?
Managing pain associated with jaw problems post-implantation can involve several strategies, including over-the-counter pain relief medications and following any specific recommendations from your healthcare provider. It’s essential to communicate any ongoing discomfort to your provider for tailored pain management solutions.
